I recently presented an expert witness bariatric surgeon for deposition in beautiful Salt Lake City, Utah.
Bariatric surgery is a field that is still rapidly developing and includes numerous procedures including lap-band, gastric sleeve, plication, bypass and imbrication. Generally speaking, bariatric procedures may help people suffering from obesity by decreasing the volume that the stomach can hold.
One of the known risks of any bariatric surgery is gastric outlet obstruction. This is a pretty easy concept to understand. After all, everything we eat has to pass through the stomach into the small intestines. If something is preventing food and liquids from passing through the stomach, it can be described as gastric outlet obstruction.
Signs and Symptoms of Gastric Outlet Obstruction
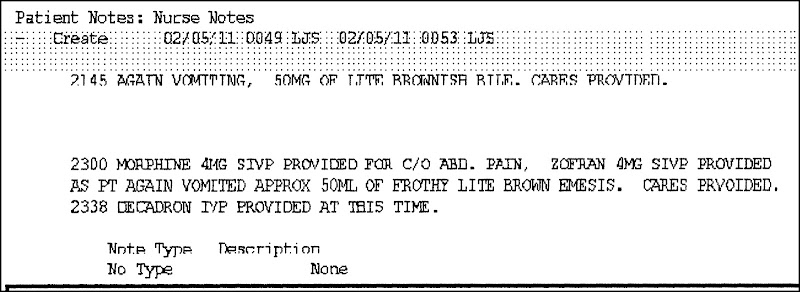
Gastric outlet obstruction is one of the known risks of any bariatric surgery. The surgeon, other doctors and the nursing staff are responsible for looking for the signs and symptoms of gastric outlet obstruction, which include nausea, vomiting and pain. And because the surgeon and other doctors are not at the hospital most of the day, a lot of that responsibility falls on the nursing staff.
At yesterday’s deposition, the attorney for Conroe Regional Medical Center (and HCA hospital) spent hours questioning the expert bariatric surgeon, trying to minimize the responsibility of the nursing staff.
Listening to the hospital’s attorney, it left me with the impression that the hospital thinks its nurses are little more than wait staff. This is wrong, though. Nurses have an independent responsibility to monitor and assess their patients and inform the doctors of their clinical findings. In other words, they have to think. And that presumes that hospitals like Conroe Regional Medical Center have actually trained the nurses properly.
To fulfill their responsibility and keep their patients safe, that means that nurses taking care of patients after a bariatric surgery need to keep an eye out for nausea and vomiting and keep the surgeon and physicians fully informed about it.
Important Key Before Discharge
It is extremely dangerous for a patient to be discharged from a hospital after a bariatric surgery without showing the ability to drink and hold down liquids without vomiting it back up for several hours (usually around 12 hours). Otherwise, there could be a dangerous gastric outlet obstruction—and the bariatric surgeon may have to take the patient back to surgery to fix it.
After the surgery, bariatric surgeons will order the nurses to start the patients on trial sips of water or warm liquids. Surgeons depend on the nurses to make sure the patients are given liquids to drink and then documenting in the medical record how much and how often the patients drink. And, of course, if the patient gets nauseated or vomits, the nurses need to record that and tell the surgeon.
This is where nursing communication to the doctors is so important—and the lack of it is so dangerous. If the surgeon orders the patient discharged, but the nurses know that he or she has not been able to hold down liquids without vomiting them up, then the nurse needs to tell the surgeon.
Most doctors only see their hospitalized patients for a few minutes a day and rely on the nursing staff to inform them of important clinical findings they have observed. When nurses drop the ball, even the best doctors are working in the dark and at a considerable disadvantage. This puts patients in needless danger.
The consequences of this medical malpractice can be dangerous and even deadly.
If you or someone you care about is hospitalized after a bariatric surgery, be sure to talk to the surgeon and the nurses about any nausea and vomiting that occurs. And be sure to speak up if there if the health care providers start talking about hospital discharge and you or your loved one has not been able to hold down liquids for several hours.
Painter Law Firm’s Houston, Texas medical malpractice attorneys are available to speak with you about your potential case involving bariatric surgery. You may reach us at 281-580-8800.