Have you ever heard the expression, "How many angels can dance on the head of a pin?" I always think of that question when considering the complexity of stroke cases under Texas law. To adapt the phrase, one might ask, "How many legal traps can dance on the head of a pin?" That's pretty much the state of stroke medical malpractice in Texas.
This article will cover some of the stroke traps and the narrow area where it may be possible to pursue a stroke medical malpractice case under existing Texas law.
Emergency rooms
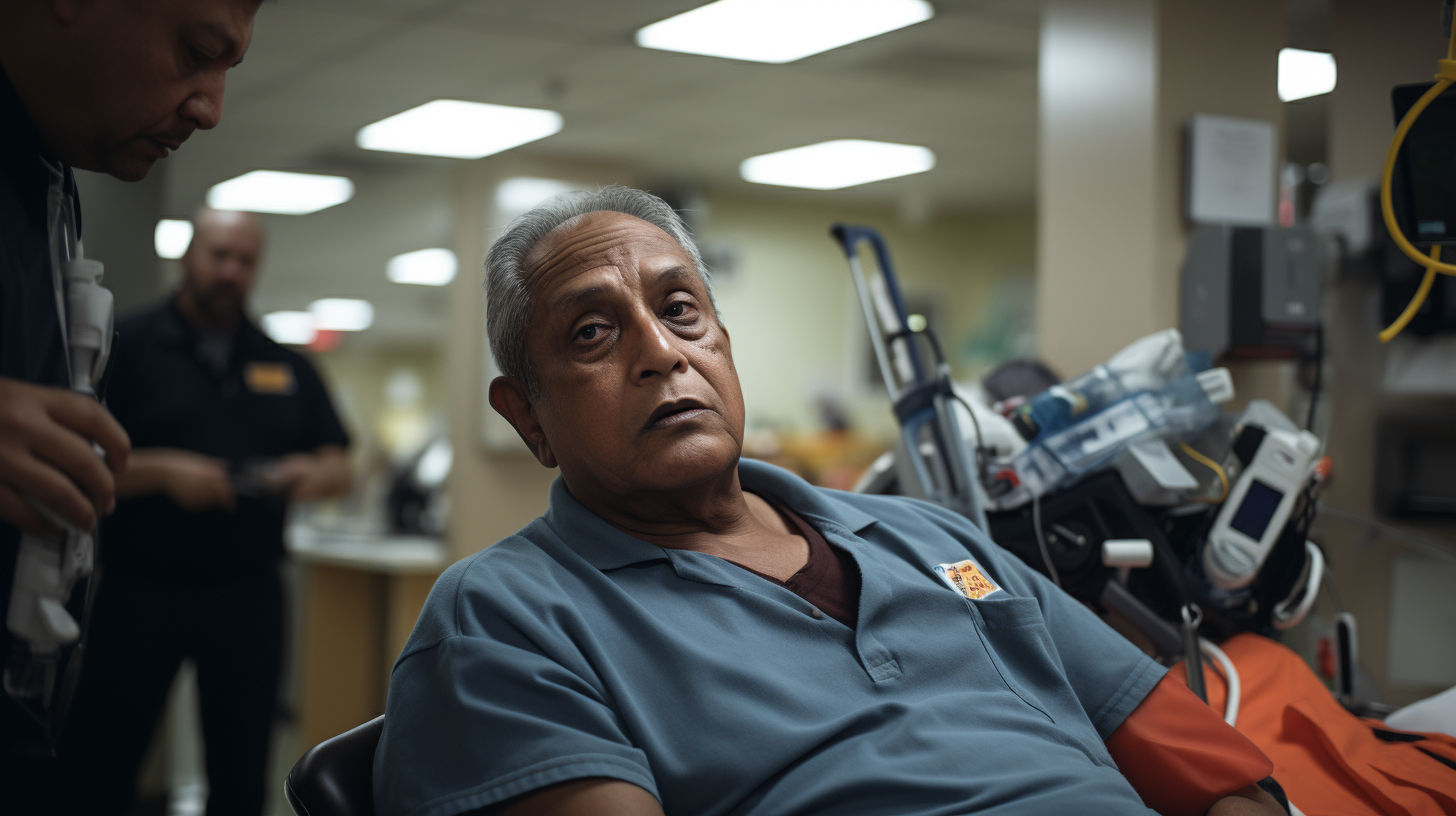
Most stroke care, including diagnosis/misdiagnosis and treatment/mistreatment, occurs in hospital emergency rooms (ERs). Texas tort reform laws that went into effect in 2003 give hospital ERs special protections when handling medical emergencies, such as strokes.
When it comes to medical malpractice cases involving hospital ERs, it's not enough that a doctor missed the diagnosis. In fact, under the tort reform willful and wanton negligence requirement, it's precisely insufficient to pursue a case.
The willful and wanton negligence standard requires the plaintiff to prove that the defendant doctor, provider, or nurse had subjective or actual awareness of a condition that posed an extreme degree of risk to a patient, but then objectively proceeded in a manner that consciously disregarded the patient's safety. You can read more about a real-world example of this in our article Texas ER botches diagnosis of man's posterior circulation stroke.
The willful and wanton negligence standard had caused us to decline potential cases where we felt we couldn't prove actual awareness by a potential defendant, including:
- A radiologist misread a CT or MRI as completely normal, when in reality there were signs of a stroke on imaging.
- A patient had clear signs and symptoms of a stroke, but none of them were documented in the medical record.
There's an interesting distinction in the law between hospital ERs and freestanding ERs. The latter didn't exist back in 2003 when the Texas legislature passed sweeping medical malpractice tort reform laws. As a result, freestanding ERs aren't referenced in the statute and aren't covered by the willful and wanton negligence standard. We believe when medical officials are not listening to the patient, other shortcuts lead to stroke misdiagnosis.
Ischemic strokes
Most strokes—around 80% of them—are ischemic strokes, or those where a blood clot breaks loose and disrupts the blood supply to the brain.
According to the American Stroke Association, the standard of care requires administration of a clot-busting drug called tissue plasminogen activator (TPA) within 4.5 hours of stroke onset. TPA busts up the clot and restores blood flow to the brain. Learn more.
To determine when the stroke began (stroke onset), ER physicians and stroke neurologists refer to the last known well. In those situations where a person woke up with stroke symptoms, it's likely impossible to say when the last known well was or when the stroke onset occurred. This means it's equally likely impossible to prove whether ER physicians and a stroke team appropriately treated an ischemic stroke patient with TPA within the 4.5-hour window because there's no evidence of when the time starting ticking.
Even when the last known well or stroke onset is known, there's another odd legal timing challenge. That's because while in a hospital setting, stroke teams will give a patient TPA within 4.5 hours after a stroke begins—and sometimes even beyond that timeframe — the legal standard is different.
When it comes to TPA administration, Texas law requires plaintiffs to prove a doubling of the benefit over not giving TPA at all. How do you prove that?
- The challenge is that some patients will improve (including recovering fully or almost fully) without receiving TPA.
- The initial studies for U.S. Food & Drug Administration (FDA) approval of TPA only show a doubling of the improvement for a narrow time group over the control group (placebo).
The conclusion of this requirement is that we're only able to consider ischemic stroke cases where there's proof that the last known well or stroke onset was no more than around 100 minutes from the time the patient went in the door of the hospital ER.
Ischemic stroke signs and symptoms
The American Stroke Association urges the public to call 911 when someone has the "FACE" warning signs of stroke. FACE stands for: Learn more.
- F = Face drooping
- A = Arm weakness
- S = Speech difficulty
- T = Time to call 911
These signs are often present in people who are having the most common type of the most common type of stroke: Anterior circulation ischemic strokes. These strokes occur when a blood clot disrupts normal blood flow to a vessel in the front of the head.
We've also handled a number of posterior circulation ischemic strokes. These occur when a blood clot interferes with blood flow to a vessel in the back of the head. The signs of an ischemic stroke in the posterior circulation are different and can include dizziness, a sense of vertigo, and a loss of balance, including the difficulty to stand or walk without assistance.
Hemorrhagic strokes
Hemorrhagic strokes, or brain bleeds, account for around 20% of all strokes.
When someone suffers from a hemorrhagic stroke and experiences poor medical treatment, it's notoriously hard to prove medical negligence. Stroke neurology experts have informed us that the current state of medicine for many hemorrhagic strokes there's no standard of care for treatment. Plus, it's often impossible to prove the essential element of causation. For most patients, the bleeding stops on its own, so it's hard to demonstrate how any treatment would've made a difference in the outcome.
What you can do
When seeking treatment for a potential stroke, be ready to describe the stroke symptoms and when they started. Remember, the last known well is an important factor. Be sure to explain your story and what happened to each physician, provider, or nurse who becomes involved in your care. Read more in our article, Stroke misdiagnosis lawsuits: When hospitals and doctors miss diagnosis of stroke, patients pay a hefty price.
We've handled lots of cases where patients with classic stroke symptoms were discharged from a stroke center ER in the same condition that brought them to the ER in the first place. I think this most often happens when a junior or less experienced doctor or provider isn't recognizing signs and symptoms or communicating them to the more senior decision maker. In these situations, keep in mind that you always have the right to ask for a second opinion, including evaluation by an attending physician.
If you've been seriously injured because of poor stroke care in Texas, then contact a top-rated experienced Texas medical malpractice law firm for a free conversation about your potential case.